KNOW YOUR PATIENTS’ BONES
BONE HEALTH
The human skeleton plays both a structural and reservoir function in the body. It enables mobility and support while also providing protection for internal organs. Bone serves as a reservoir for essential minerals such as calcium and phosphorous. The skeleton is an active organ made up of tissues and cells which are in a constant state of flux and impact bone shape, size, and position throughout life.
Bone growth and development occurs throughout one’s lifetime, with most bone mass acquired during childhood and teenage years. Bone formation outpaces bone resorption until one reaches peak bone mass, typically in the 20’s through age 30. Around the mid 30’s, the scales tip and bone resorption slowly starts to exceed bone formation which leads to age-related bone loss. Diet and exercise play key roles in managing age-related bone loss. Excess loss of bone mineral mass can lead to conditions such as Osteopenia and Osteoporosis later in life.^^
CALCIUM AND VITAMIN D
Calcium is the most abundant mineral in the body with 99% of it stored in the body’s bones and teeth. Vitamin D is critical for enabling normal bone mineralization through its role in promoting calcium absorption from the gastrointestinal tract. There is no question that calcium and vitamin D are essential for keeping bones healthy and moving. However, nutrition intake surveys in the US continue to show that Americans fall short on adequate consumption of these important nutrients. The 2010 Dietary Guidelines for Americans identified both of these nutrients as under-consumed by the general population and thus deemed them to be nutrients of public health concern.
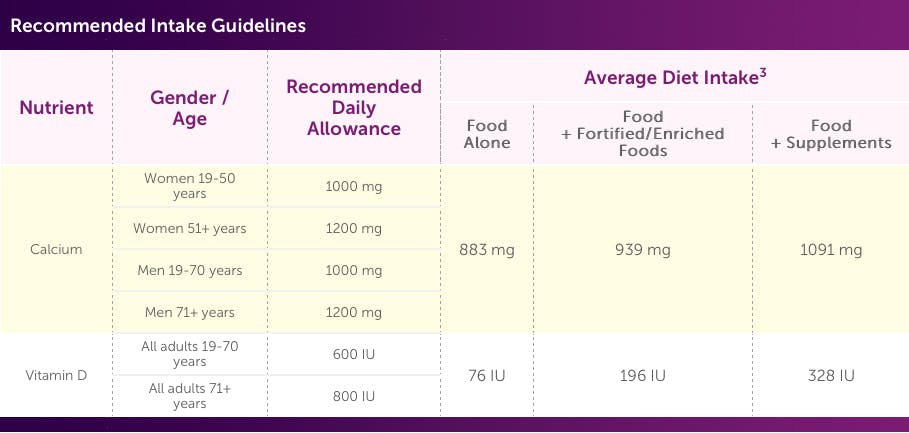
Below are recommended intake guidelines for these key nutrients from the Institute of Medicine’s Dietary Reference Intakes compared to average dietary intake found in the National Health and Nutrition Examination Surveys.3
ROLE OF ESSENTIAL MINERALS IN BONE HEALTH
Bone is made up of ~2/3 minerals and ~1/3 collagen. This unique combination of minerals and protein (collagen) allows for the dual action of bone strength and flexibility. Consider that a structure made only of minerals would essentially be brittle and break easily because there is no flexibility, while a structure made only of protein would be soft and bend too easily. While calcium and vitamin D are important nutrients for bone strength, minerals such as magnesium, copper, manganese, and zinc play a role in supporting collagen formation in the body. Additionally, collagen has great tensile strength and not only provides support to bones, but to the many other organs and tissues in which it is also contained, including cartilage, ligaments, tendons, and skin.
Age-related changes affect absorption of calcium and maintenance of healthy collagen, thus adequate intake of calcium, vitamin D, and key collagen supporting minerals through diet and/or supplementation is important for good bone health.
BONE HEALTH
IS OSTEOPOROSIS MEDICINE ENOUGH?
Start your bone health program off right by getting enough calcium and vitamin D. If you're not getting enough calcium from food, then your body will steal it from your bones. And inadequate levels of calcium can lead...

ADDITIONAL BONE HEALTH RESOURCES:
Article: Is Osteoporosis Medicine Enough?
Bone Health Central: Interactive Tools, Articles, and Health Tips
References:
1. Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B. Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA. 2005;293(18):2257-2264.
2. Dietary Guidelines for Americans 2010, Chapter 4. Available at: http://www.cnpp.usda.gov/publications/dietaryguidelines/2010/policydoc/chapter4.pdf
3. Fulgoni, et al. Food, Fortificants, and Supplements: Where do Americans Get their Nutrients? The Journal of Nutrition 2011
4. Institute of Medicine. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington DC: National Academy Press; 2001.
5. Institute of Medicine. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington DC, National Academy Press; 2000:190-249.
6. Lodish H, Berk A, Zipursky SL, Matsudaira P, Baltimore D, Darnell J. Molecular Cell Biology. 4th ed. New York: W. H. Freeman; 2000.
7. Nordin BE, Need AG, Chatterton BE, Horowitz M, Morris HA. The relative contributions of age and years since menopause to postmenopausal bone loss. J Clin Endocrinol Metab. 1990;70:83-88.
8. Office of the Surgeon General (US). Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville (MD): Office of the Surgeon General (US); 2004. 2, The Basics of Bone in Health and Disease. Available from: http://www.ncbi.nlm.nih.gov/books/NBK45504/
9. Prince RL, Devine A, Dhaliwal SS, Dick IM. Effects of calcium supplementation on clinical fracture and bone structure: results of a 5-year, double-blind, placebo-controlled trial in elderly women. Arch Intern Med. 2006;166(8):869-875.
10. Saltman PD, Strause LG. The role of trace minerals in osteoporosis. J Am Coll Nutr. 1993;12(4):384-389.


